Tips to Manage the Symptoms of Diabetic Neuropathy
Diabetic neuropathy, a common complication of diabetes, refers to nerve damage caused by prolonged exposure to high blood sugar levels. This condition can affect various body parts, leading to pain, tingling, numbness, and weakness, particularly in the extremities. Managing diabetic neuropathy is crucial for improving the quality of life for those affected. This comprehensive guide will explore various tips and strategies to manage the symptoms of diabetic neuropathy effectively.
Understanding Diabetic Neuropathy: A Brief Overview
Before delving into management strategies, it’s essential to have a basic understanding of diabetic neuropathy. Diabetes, a condition denoted by elevated blood sugar levels, can damage the nerves over time. This damage often begins in the peripheral nerves transmitting signals between the central nervous system and the rest of the body. Fortunately, you can now use a diabetic nerve pain cream to help manage the discomfort associated with diabetic neuropathy. These creams are formulated with ingredients designed to provide targeted relief to the affected areas, offering a potential complement to other management strategies. Diabetic neuropathy can manifest in different forms:
- Peripheral Neuropathy: Affects the nerves in the feet and legs, leading to pain, tingling, and numbness.
- Autonomic Neuropathy: Involves the nerves that control involuntary bodily functions, resulting in digestive problems, blood pressure irregularities, and sexual dysfunction.
- Proximal Neuropathy: Affects the nerves in the thighs, hips, or buttocks, causing muscle weakness and pain.
- Focal Neuropathy: Results in the sudden, localized onset of pain or muscle weakness, often in the eyes, facial muscles, or hands.
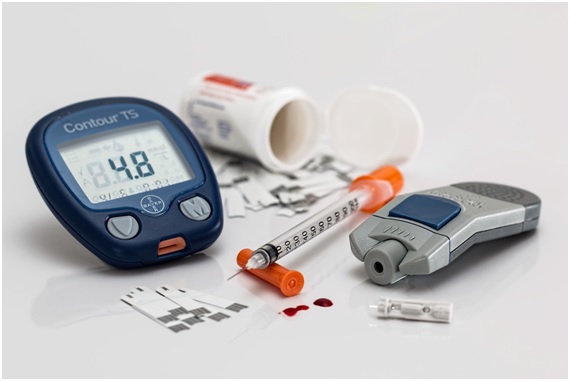
Blood Sugar Management: The Foundation of Neuropathy Care
The cornerstone of managing diabetic neuropathy lies in effectively controlling blood sugar levels. High and fluctuating blood glucose can exacerbate nerve damage and intensify symptoms. Consider the following tips for maintaining optimal blood sugar levels:
- Regular Monitoring: Monitor blood sugar levels regularly as advised by your healthcare provider. This helps identify trends and make necessary adjustments to your diabetes management plan.
- Medication Adherence: Take prescribed diabetes medications consistently and as directed. Adhering to your medication regimen is crucial for stabilizing blood sugar levels.
- Balanced Diet: Adopt a balanced and nutritious diet. Focus on whole foods, fruits, vegetables, lean proteins, and complex carbohydrates. Consult a registered dietitian for them to create a personalized meal plan for you.
- Physical Activity: Engage in routine physical activity to help control blood sugar levels. Consult your healthcare practitioner before starting a new exercise regimen to ensure it’s safe for your health.
Pain Management Strategies
Pain is a common and often challenging symptom of diabetic neuropathy. Effectively managing pain is crucial for improving overall well-being. Consider the following pain management strategies:
- Medications: Over-the-counter pain relievers like acetaminophen or prescription medications may be recommended. Discuss the appropriate options with your healthcare provider.
- Topical Treatments: Creams, capsaicin patches or lidocaine may relieve localized pain. Always follow the instructions and consult your healthcare provider before using these products.
- Mind-Body Techniques: Meditation, deep breathing exercises, and guided imagery can help manage pain by promoting relaxation and reducing stress.
- Physical Therapy: Consult a physical therapist for exercises and stretches that can aid in alleviating pain and improving mobility.
Foot Care: Preventing Complications
Peripheral neuropathy often affects the feet, making proper foot care crucial for preventing complications such as infections and ulcers. Inspect your feet daily for any wounds or changes in color. Promptly address any issues and consult your healthcare provider if you notice abnormalities. Wear comfortable shoes providing adequate support and do not cause friction or pressure points. Avoid going barefoot, especially in areas where injury is more likely. Keep the skin on your feet moisturized to prevent dryness and cracking. However, avoid applying moisturizer between the toes to prevent fungal infections. Trim your toenails straight across and avoid cutting into the corners to reduce the risk of ingrown toenails. You may want to speak to a specialist that deals with peripheral neuropathy Owasso, or a nearby alternative to see if they have any useful advice.
Neuropathy-Friendly Exercises
Regular exercise is beneficial for overall health, helping manage the symptoms of diabetic neuropathy. However, choosing activities that are safe for your condition is essential. Opt for low-impact exercises, which include walking, swimming, or cycling. These activities are gentle on the joints, improving circulation without putting excessive stress on the feet. Incorporate stretching exercises into your workout routine to improve flexibility and reduce muscle tightness. Consult with a physical therapist for personalized stretching recommendations. Include strength training exercises to maintain muscle mass and improve overall strength. Start with light weights, focusing on proper form—practice balance exercises, reducing the risk of falls. Tai Chi or yoga can be particularly beneficial for enhancing balance and flexibility.
Lifestyle Modifications for Neuropathy Management
Certain lifestyle modifications can contribute to better symptom management and an improved quality of life. Consider the following tips:
- Smoking Cessation: Smoking can restrict blood flow and worsen nerve damage. Quitting smoking is good for your health and can positively impact neuropathy symptoms.
- Alcohol Moderation: Excessive alcohol consumption can exacerbate neuropathy symptoms. If you choose to drink, do so in moderation, following the guidelines recommended by healthcare professionals.
- Temperature Awareness: Diabetic neuropathy can affect your ability to sense temperature changes. Avoid extreme temperatures and use protective measures, such as wearing appropriate clothing in cold weather.
- Stress Management: Chronic stress can exacerbate neuropathy symptoms. Incorporate stress-management techniques such as mindfulness, meditation, or hobbies that promote relaxation.
Regular Medical Check-ups and Communication with Healthcare Providers
Consistent communication with your healthcare team is crucial for effectively managing diabetic neuropathy. Schedule regular check-ups and promptly report any changes in symptoms. Provide detailed information about changes in symptoms, including the nature and intensity of pain, any new sensations, or difficulties with mobility. Work closely with your healthcare practitioner to adjust medications as needed. Changes in symptoms or overall health may require modifications to your treatment plan. Stay up-to-date with recommended screenings for diabetes-related complications, including eye exams, kidney function tests, and cardiovascular assessments. Participate actively in decisions regarding your healthcare. Discuss treatment options, potential side effects, and any concerns.
Diabetic neuropathy poses challenges, but with proactive management strategies, individuals can lead fulfilling and active lives. Remember that the key lies in a comprehensive approach that addresses blood sugar control, pain management, lifestyle adjustments, and regular communication with healthcare providers. By adopting these tips and working collaboratively with your healthcare team, you can navigate the complexities of diabetic neuropathy with resilience and empower yourself to lead a life that is not defined by the condition. Always remember that you are not alone on this journey; support is available to help you effectively manage the symptoms and embrace a healthier, more vibrant future.
Read Also: Zintego’s Invoice Template, Receipt Maker, and Invoice Generator